Preterm nutritional needs and feeding challenges: a guide for healthcare professionals
Several studies have shown that growth failure of preterm infants affects health in later life and compromises brain development1,2. Therefore, avoiding growth failure is a central challenge in preterm nutrition1-3.

Please log in to access this content
Simply log in or register to Nutricia Academy today to access this content as well as a host of other trusted education resources.

Preventing growth failure
Preterm infants have increased nutrient requirements to achieve the growth velocity of a child growing in its mother’s womb4,5. These requirements are much higher than those of a term born peer4-6. Medical associations such as the European Society for Gastroenterology, Hepatology, and Nutrition (ESPGHAN)6 and American Academy of Pediatrics (AAP)7 as well as neonatal experts⁸ address these requirements by giving specific recommendations for premature infants born weighing less than 1000g, less than 1500g and less than 1800g. All these associations acknowledge that protein is a key nutrient in avoiding growth failure as long as enough energy is provided6-8.
In support of optimal growth and development, preterm nutrition should address:
- High nutritional needs and growth velocity versus difficulties of enteral intake
- Instable metabolsim due to immature gastrointestinal development
- Immature / compromised immune system
- Delayed colonisation and compromised microbiota development
- Sensitive phase of brain development
Breast is best
In line with the World Health Organisation (WHO) we believe that human milk is the best nutrition for preterm infants9. Breastfeeding and human milk (HM) are the preferred feeding mode and nutrition for every infant10-13.
The composition of HM is highly variable and tailored to the personal nutritional needs of an infant14-16. For preterm infants on parenteral feeds, trophic feeding with HM soon after birth is recommended to prepare the intestine for enteral feeding3,11,12.
Maternal human milk benefits
Beyond the benefits of breastfeeding known for term infants17, providing HM to premature infants:
- offers immune protection against infection3,11,12
- reduces the risk of necrotising enterocolitis (NEC)3,11,12
- prepares the gut for enteral feeding3,11,12
- supports healthy gut development3,11,12
- provides enzymes for fat absorption12
- is associated with improved neurocognitive development3,11,12
- is tolerated well3,11,12, and personalised to the mother-infant15,16
Colostrum, a pre-milk fluid rich in immunoglobulins and immune cells that is produced during the first 24–48 hours postpartum, is especially important for immune protection and gut maturation and should never be discarded12.
Donor human milk
If own mothers milk (OMM) is not available donor human milk (DHM) from milk banks is the next preferred alternative for preterm infant feeding13. However, as with OMM, DHM is not nutrient enriched enough to meet the high requirements of extreme and very premature infants and fortification i.e. adding macro- and micronutrients to HM or a multicomponent Human Milk Fortifier (HMF) is required6,8,18.
Fortification
HM fortification is associated with improved growth and brain development3,6,8,10-13,18. Infants born weighing less than 1800g are recommended to receive fortified HM enriched in energy, macronutrients, minerals, and vitamins6,8 to achieve growth rates similar to those of the fetus. However, infants born weighing less than 1000 g and/or those born small-for-gestational age may need an even faster weight gain for recovering growth19,20 and have therefore even higher protein and energy needs6,8,18,19.
Human milk is the preferred nutrition for preterm infants. However, fortification is recommended for preterm infants <1800g to ensure the required nutrients are received alongside all HM associated benefits for healthy growth and development.
Feeding challenges
Avoiding growth failure by meeting the high energy and protein needs is challenging: enteral feeding commonly takes place through naso-gastric tubes because of feeding difficulties4. The feed needs to be highly concentrated because of small stomach volumes that limit intake, but also well tolerated4-6.
Physiology
An immature gut physiology affects growth. Healthy growth can only be achieved with an intact healthy gut that is capable of digesting and absorbing the provided nutrients, and a metabolism prepared to use nutrients effectively4.
The colonic microbiota, compromised in preterm infants because of prophylactic use of antibiotics and pathogens in the hospital environment, play an important role in maintaining a healthy gastrointestinal environment for digestion of nutrients21,22.
Intestinal microbiota also plays a vital role in the immune system21, helping to reduce the risk of infection and necrotising enterocolitis, which compromise survival and/ or growth22.
As such, providing appropriate nutrition to meet the high nutrient and energy requirements and support the colonisation of healthy intestinal microbiota is essential to improve gut and immune health, which provides the platform for adequate growth. Together, these factors create an environment for long term health.
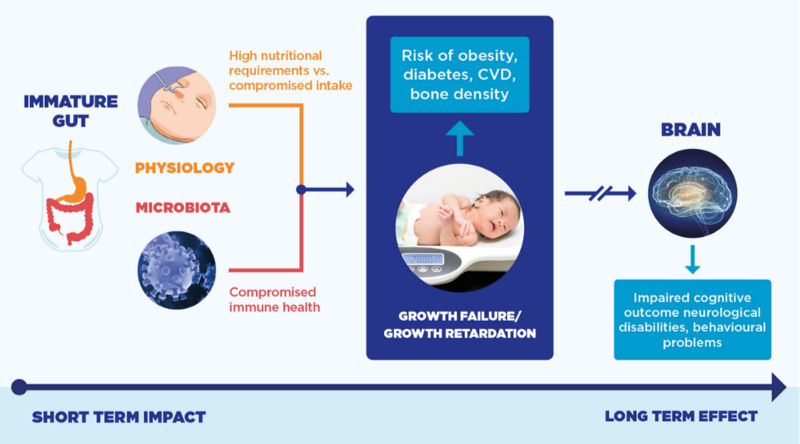
Adequate growth is a major challenge for preterm infants. It is affected by an immature gut and metabolic physiology and as a consequence inadequate intake, digestion, uptake and usage of the nutrients. Moreover suboptimal intestinal microbiota and an immature immune system may play a role in the risk of infection and necrotising enterocolitis, further compromising growth. Together the factors/processes leading to growth failure also impact/ compromise brain development.
40 years of early life science
Nutricia has over 40 years of breast milk expertise with a dedicated team of around 250 specialist scientists collaborating with hospitals, laboratories and universities worldwide to ensure we’re leaders in this field. At Nutricia, science is at the heart of our nutrition and health commitment to help healthcare professionals support parents during the first 1,000 days. Our research and innovation delivers evidence-based nutritional solutions to support a child’s lifelong health, combining our Early Life Nutrition expertise with years of professional experience to develop a portfolio of products to support the nutritional needs of mums, mums-to-be and their babies.
- Ehrenkranz et al. (2006) Pediatrics . 117(4): 1253–1261.
- Stephens et al. (2009) Pediatrics. 123(5): 1337–1343.
- Ziegler. (2015) J Pediatr Gastroenterol Nutr. 61 Suppl 1: S3.
- Klein (Ed.). (2002) J Nutr. 132(6 Suppl 1): 1395S-1577S.
- Clark et al. (2003) Pediatrics. 111(5 Pt 1): 986–990.
- Agostoni et al. (2010) J Pediatr Gastroenterol Nutr. 50: 85–91.
- AAP Committee on Nutrition. (2014) Section II: Feeding the preterm infant. 83–110. In: Kleinman & Greer (Eds.) Pediatric Nutrition. 7th Edition. Elk Grove Village, IL, USA.
- Koletzko-Uauy-Pointdexter. (2014) 110: 297–299. Recommended nutrient intake levels for stable, fully enterally fed very low birth weight infants. In: In: Koletzko-Uauy-Pointdexter (Eds.). Nutritional care of preterm infants: Scientifi c basis and practical guidelines. Karger, Basel, Switzerland.
- World Health Organization’s infant feeding recommendation (http://www.who.int/nutrition/topics/infantfeeding_recommendation/en/) last accessed: July 2018.
- Howson, Kinney, Lawn (Eds.). (2012) Born Too Soon: The Global Action Report on Preterm Birth. World Health Organisation. Geneva, Switzerland.
- Moro et al. (2015) J Pediatr Gastroenterol Nutr. 61 Suppl 1: S16–19
- Tudehope. (2013) J Pediatr 162:S17-S25.
- AAP (2012). Pediatrics 129(3): e827–2841.
- Lonnerdal. (2013) J Paediatr Child Health. 49 Suppl 1: 1–7.
- Hassiotou et al. (2013) Clin Transl Immunology. 2(4): e3.
- Powe et al. (2010) Am J Hum Biol. 22(1): 50–54.
- Hennet & Borsig. (2016) Trends Biochem. Sci 41(6): 508–518.
- Arslanoglu. (2015) J Pediatr Gastroenterol Nutr. 61 Suppl 1: S4–5.
- Ziegler. (2015) Nestle Nutr Inst Workshop. Ser 81: 135–143.
- Clark et al. (2014) Clin Perinatol. 41(2): 295–307.
- Jeurink et al. (2013) Am J Clin Nutr. 98(2): 572S-577S.
- Neu. (2014) 110: 253–263. In: Koletzko-Uauy-Pointdexter (Eds.). Nutritional care of preterm infants: Scientifi c basis and practical guidelines. Karger, Basel, Switzerland.



